In the realm of medical science, few stories are as extraordinary as that of Tim Friede, a self-taught snake expert who willingly subjected himself to the venom of some of the world’s deadliest snakes over nearly two decades. What began as a seemingly reckless endeavor has now led to a groundbreaking discovery that could revolutionize the treatment of snakebites globally. This remarkable journey, spearheaded by immunologist Jacob Glanville, has culminated in the development of an antivenom that offers protection against bites from 19 species of venomous snakes—a feat that could save countless lives.
The Unlikely Collaboration
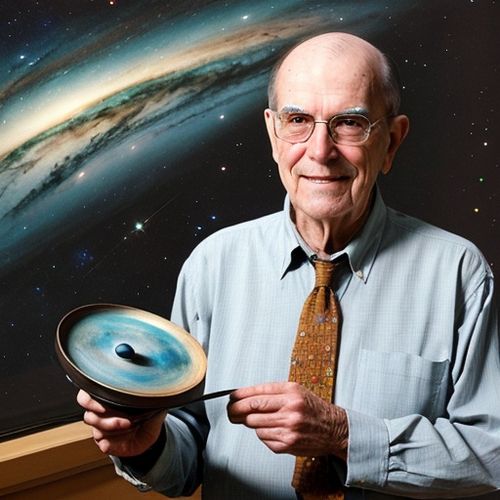
In 2017, Jacob Glanville stumbled upon media reports about Tim Friede, a California-based snake expert who had injected himself with venom from cobras, mambas, and rattlesnakes hundreds of times. While the news articles sensationalized Friede’s actions, Glanville saw something more: a unique opportunity to advance medical science. "I was like there’s a diamond in the rough here," Glanville recalled. He reached out to Friede, who had meticulously documented his exposure to various snake venoms over 17 years and nine months. "Finally, I’ve been waiting for this call," Friede responded when Glanville asked for a blood sample.
The Quest for a Universal Antivenom
Friede’s blood held the key to a potential breakthrough. By exposing himself to diverse snake venoms, he had developed antibodies that were effective against multiple neurotoxins. Glanville and his team, including Peter Kwong from Columbia University’s Vagelos College of Physicians and Surgeons, set out to isolate these antibodies and develop a universal antivenom. Their goal was ambitious: to create a treatment that could neutralize venom from a wide range of snake species, addressing a critical need in global health.
Snakebites are a significant public health issue, particularly in the developing world. The World Health Organization estimates that snakebites kill approximately 200 people daily and leave 400,000 with disabilities each year. Traditional antivenom production, which involves milking venom from snakes and injecting it into animals to elicit an immune response, is laborious, error-prone, and often results in severe side effects. Glanville recognized that Friede’s unique immunity could offer a safer and more effective alternative.
The Science Behind the Breakthrough
The research team isolated antibodies from Friede’s blood that reacted with neurotoxins from 19 snake species, including coral snakes, mambas, cobras, taipans, kraits, and others. These antibodies were tested in mice poisoned by venom from each species. The results were remarkable: a cocktail of two antibodies and a small-molecule drug called varespladib provided 100% protection against venom from 13 species and partial protection (20% to 40%) for the remaining six.
The first antibody, LNX-D09, protected mice from a lethal dose of whole venom from six snake species. Adding varespladib extended protection to three more species. Finally, a second antibody, SNX-B03, broadened the protection to all 19 species tested. This combination of human-derived antibodies and a small-molecule drug represents a significant advancement over traditional antivenom production methods.
The Promise of a Safer, More Effective Treatment
The potential impact of this discovery is immense. Steven Hall, a snakebite pharmacologist at Lancaster University in the United Kingdom, described the research as a "very clever and creative way" to develop an antivenom. Unlike traditional antivenoms, which are derived from animal blood and can cause allergic reactions, the human origin of the antibodies in this cocktail is likely to result in fewer side effects.
"This is impressive for the fact that this is done with one or two antibodies, plus a small-molecule drug, and that increases the number of species versus a regular antidote," Hall said. "If it makes it into the clinic, it would be revolutionary. It would completely change the field in terms of snakebite treatment."
Looking Ahead
While the antivenom has not yet been tested in humans, the research team is optimistic about its potential. The next steps include further clinical trials and field research, particularly in regions where snakebites are prevalent. The team is also exploring whether additional antibodies identified in Friede’s blood could offer protection against other venomous snake families, such as viperids.
Kwong emphasized that the ultimate goal is to develop a single, pan-antivenom cocktail that could be used globally. Alternatively, they may create two specialized cocktails—one for elapids and another for viperids—depending on the snake species prevalent in different regions. Field research in Australia, where only elapid snakes are found, is also planned to test the antivenom on dogs bitten by snakes.
A Cautionary Tale and a Call to Action
Despite the promising results, Glanville and his team strongly discourage others from attempting to replicate Friede’s dangerous experiments. "Snake venom is dangerous," Glanville warned. Friede himself gave up immunizing himself with snake venom in 2018 after several close calls and now works with Glanville’s biotechnology company, Centivax.
The development of this antivenom is not just a scientific achievement; it is a testament to the potential of unconventional approaches and the importance of supporting innovative research. As the world grapples with the devastating impact of snakebites, the work of Glanville, Friede, and their colleagues offers a glimmer of hope for a safer, more effective treatment.
The journey from Friede’s self-experimentation to the development of a groundbreaking antivenom is a remarkable story of scientific ingenuity and perseverance. By harnessing the power of human-derived antibodies and combining them with advanced pharmaceuticals, the research team has taken a significant step towards addressing a critical global health challenge. While much work remains to be done, the potential for this antivenom to save lives and reduce the burden of snakebites is truly revolutionary.

By Sophia Lewis/May 6, 2025
By Olivia Reed/May 6, 2025

By William Miller/May 6, 2025

By Eric Ward/May 6, 2025

By John Smith/May 6, 2025

By Rebecca Stewart/May 6, 2025

By Benjamin Evans/May 6, 2025
By Eric Ward/May 6, 2025

By Eric Ward/May 6, 2025

By Daniel Scott/May 6, 2025

By Benjamin Evans/May 6, 2025
By Elizabeth Taylor/May 6, 2025

By James Moore/May 6, 2025

By Victoria Gonzalez/May 6, 2025

By Sophia Lewis/May 6, 2025

By Laura Wilson/May 6, 2025

By Olivia Reed/May 6, 2025

By David Anderson/May 6, 2025

By Olivia Reed/May 6, 2025
By Sophia Lewis/May 6, 2025